Everything You Need to Know About Artificial Insemination
Infertility and Artificial Insemination
When you and your partner talk to a doctor about getting help for infertility, he may suggest a technique called "artificial insemination." It's a simple procedure with few side effects, and it can help some couples who haven't been able to get pregnant.
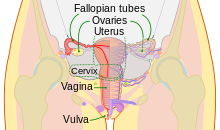
In artificial insemination, a doctor inserts sperm directly into a woman's cervix, fallopian tubes, or uterus. The most common method is called "intrauterine insemination (IUI)," when a doctor places the sperm in the uterus.
Why is this helpful? It makes the trip shorter for the sperm and gets around any obstructions. Your doctor may suggest this method first as a treatment for infertility.
What Type of Infertility Can Artificial Insemination Treat?
The procedure can be used for many kinds of fertility problems. In cases involving male infertility, it's often used when there's a very low sperm count or when sperm aren't strong enough to swim through the cervix and up into the fallopian tubes.
Why use it?
 Artificial insemination can help people who are trying to treat infertility.
Artificial insemination can help people who are trying to treat infertility.
Artificial insemination can benefit couples or individuals with a range of needs.
In the United States, 6 per cent of women aged 15 to 44 years are unable to conceive or maintain a pregnancy after one year of unprotected sex.
The Centers for Disease Control and Prevention (CDC) suggest that a woman should consider seeing a fertility doctor to discuss treatment if she is:
- Unable to conceive within one year of trying
- prone to irregular periods
- over 35 years of age and trying to conceive
Doctors also recommend fertility treatment if a woman has two or more spontaneous miscarriages.
IUI can help in the following medical situations:
- IUI can help support a couple that produces healthy sperm and eggs but is unable to have intercourse, possibly due to a medical condition, such as erectile dysfunction.
- In women with cervical factor infertility, the cervix either does not produce the mucus that helps sperm travel to the womb, or the mucus contains a substance that kills the sperm. Artificial insemination can help bypass this problem.
- Endometriosis causes the cells from the womb lining start to grow outside the womb, for example, in the ovaries or the fallopian tubes. Artificial insemination can be successful in mild to moderate cases of endometriosis. Many women with endometriosis can conceive naturally.
- In rare cases, a woman may have an allergic reaction to certain proteins in sperm or semen. Artificial insemination can remove most of these before applying the sperm.
- Some men are unable to produce enough sperm for successful fertilization, or their sperm may not be sufficiently motile. This means the sperm cannot move towards the egg effectively.
- Certain medical treatments carry infertility as a risk, such as radiation therapy.
Before the treatment, a man can freeze some of his sperm for future use in artificial insemination.
In some couples, there is no clear reason for infertility, but the doctor may recommend IUI regardless.
Techniques
Semen used is used either fresh, raw, or frozen. Where donor sperm is supplied by a sperm bank, it will always be quarantined and frozen and will need to be thawed before use. When an ovum is released, semen is introduced into the woman's vagina, uterus or cervix, depending on the method being used.
Sperm is occasionally inserted twice within a 'treatment cycle'.
Can it be done at home?
Some women may choose home insemination. Most commonly, home inseminations are ICI procedures.
Some of the benefits of an at-home artificial insemination are that a woman can be in the privacy of her own home. Most commonly, a practitioner such as a midwife will use an unwashed specimen that’s obtained directly and immediately from a man.
At-home inseminations aren’t as regulated as they are at a medical office. For this reason, it’s important that a woman or couple thoroughly discuss the procedure and its risks and benefits with the person performing the insemination. A home environment increases the risk of infection over a clinical environment.
People can also purchase at-home insemination kits. These kits come with containers for semen and syringes to collect the semen and insert it through the vagina. While the procedure is fairly straightforward, it may be difficult for a woman to perform on herself. It can take several attempts before a successful conception.
Risks
There are a few risks when undergoing artificial insemination.
The risk of conceiving twins or triplets increases if a woman receives IUI at the same time as other fertility medication, such as gonadotrophin.
A pregnancy with more than one fetus increases the chances of complications, such as premature birth or miscarriage.
Nowadays, doctors only prescribe fertility medication when there are difficulties with ovulation, or producing the egg cells from which an embryo develops.
Ovarian hyperstimulation syndrome (OHSS) can the ovaries to swell after combining fertility medication and IUI. It is rare, and symptoms are usually mild-to-moderate, but it can sometimes have serious complications.
In mild cases of OHSS, symptoms include bloating, slight abdominal pain, and possibly nausea and vomiting. More severe cases may feature dehydration, chest pain and shortness of breath.
Staying hydrated and taking paracetamol normally alleviates the pain, but more severe cases may require hospital treatment.
Pregnancy rate
The pregnancy or success rates for artificial insemination are 10 to 15% per menstrual cycle using ICI, and 15–20% per cycle for IUI. In IUI, about 60 to 70% have achieved pregnancy after 6 cycles.
However, these pregnancy rates may be very misleading, since many factors, including the age and health of the recipient, have to be included to give a meaningful answer, e.g. definition of success and calculation of the total population. For couples with unexplained infertility, unstimulated IUI is no more effective than natural means of conception.
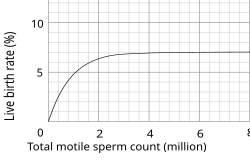
The pregnancy rate also depends on the total sperm count, or, more specifically, the total motile sperm count (TMSC), used in a cycle. The success rate increases with increasing TMSC, but only up to a certain count, when other factors become limiting to success. The summed pregnancy rate of two cycles using a TMSC of 5 million (maybe a TSC of ~10 million on the graph) in each cycle is substantially higher than one single cycle using a TMSC of 10 million. However, although more cost-efficient, using a lower TMSC also increases the average time taken to achieve pregnancy. Women whose age is becoming a major factor in fertility may not want to spend that extra time.
Samples per child
The number of samples (ejaculates) required to give rise to a child varies substantially from person to person, as well as from clinic to clinic. However, the following equations generalize the main factors involved:
For intracervical insemination:
- N is how many children a single sample can give rise to.
- Vs is the volume of a sample (ejaculate), usually between 1.0 mL and 6.5 mL
- c is the concentration of motile sperm in a sample after freezing and thawing, approximately 5–20 million per ml but varies substantially
- rs is the pregnancy rate per cycle, between 10% to 35%
- nr is the total motile sperm count recommended for vaginal insemination (VI) or intra-cervical insemination (ICI), approximately 20 million pr. ml.
The pregnancy rate increases with increasing number of motile sperm used, but only up to a certain degree, when other factors become limiting instead.
show
Derivation of the equation (click at right to view)
With these numbers, one sample would on average help giving rise to 0.1–0.6 children, that is, it actually takes on average 2–5 samples to make a child.
For intrauterine insemination, a centrifugation fraction (fc) may be added to the equation:
- fc is the fraction of the volume that remains after centrifugation of the sample, which may be about half (0.5) to a third (0.33).
On the other hand, only 5 million motile sperm may be needed per cycle with IUI (nr=5 million)
Thus, only 1–3 samples may be needed for a child if used for IUI.
History
The first reported case of artificial insemination by donor occurred in 1884: Dr William H. Pancoast, a professor in Philadelphia, took sperm from his "best looking" student to inseminate an anaesthetized woman. The woman was not informed about the procedure, unlike her infertile husband. The case was reported 25 years later in a medical journal. The sperm bank was developed in Iowa starting in the 1920s in research conducted by the University of Iowa medical school researchers Jerome Sherman and Raymond Bunge.
In the 1980s, direct intraperitoneal insemination (DIPI) was occasionally used, where doctors injected sperm into the lower abdomen through a surgical hole or incision, with the intention of letting them find the oocyte at the ovary or after entering the genital tract through the ostium of the fallopian tube.
Social implications
One of the key issues arising from the rise of dependency on assisted reproductive technology (ARTs) is the pressure placed on couples to conceive; 'where children are highly desired, parenthood is culturally mandatory, and childlessness socially unacceptable'.
The medicalization of infertility creates a framework in which individuals are encouraged to think of infertility quite negatively. In many cultures donor insemination is religiously and culturally prohibited, often meaning that less accessible "high tech" and expensive ARTs, like IVF, are the only solution.
An over-reliance on reproductive technologies in dealing with infertility prevents many – especially, for example, in the "infertility belt" of central and southern Africa – from dealing with many of the key causes of infertility treatable by artificial insemination techniques; namely preventable infections, dietary and lifestyle influences.
If good records are not kept, the offspring when grown up risk accidental incest.
Morality in Christianity
An Anglican writer says that "To achieve union but not children by means of contraceptives and to achieve children but not union by means of artificial insemination are both equally wrong." Heterosexual intercourse is viewed by the Catholic Church as an act meant to be experienced only by married couples; it is viewed as a physical representation of the spiritual unity of marriage between a husband and wife. According to the Catechism of the Catholic Church, artificial insemination "dissociates the sexual act from the procreative act. The act which brings the child into existence is no longer an act by two persons giving themselves to one another, but one that 'entrusts the life and identity of the embryo into the power of doctors and biologists and establishes the domination of technology over the origin and destiny of the human person. Such a relationship of domination is, in itself, contrary to the dignity and equality that must be common to parents and children'".
Legal restrictions
Some countries restrict artificial insemination in a variety of ways. For example, some countries do not permit AI for single women, and some Muslim countries do not permit the use of donor sperm. As of May 2013, the following European countries permit medically assisted AI for single women:
 Armenia
Armenia Belarus
Belarus Belgium
Belgium Bulgaria
Bulgaria Cyprus
Cyprus Denmark
Denmark Estonia
Estonia Finland
Finland Germany
Germany Greece
Greece Hungary
Hungary Iceland
Iceland Ireland
Ireland Latvia
Latvia Macedonia
Macedonia Moldova
Moldova Montenegro
Montenegro Netherlands
Netherlands Romania
Romania Russia
Russia Spain
Spain Ukraine
Ukraine United Kingdom
United Kingdom
In animals
AI is useful for pets, livestock, endangered species, and animals in zoos or marine parks difficult to transport.



















Hey, nice great post, Thanks for sharing this helpful information, next time come back again for more interesting information. Keep it up! Sago - Sperm Donor Cyprus
ReplyDelete